Game-changing gene found in animal study could switch off cancer for life
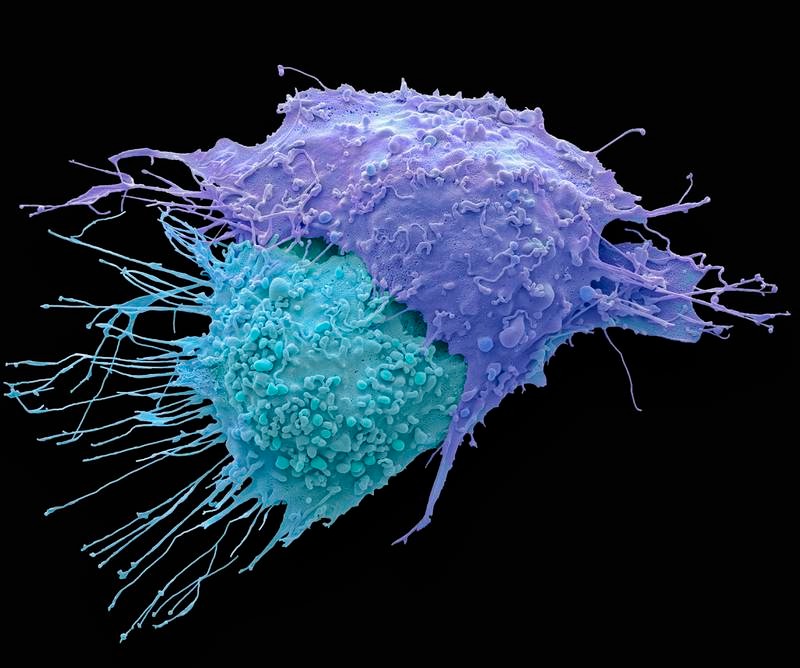
Image: Collected
Researchers have identified a potential game-changer in the quest for more effective cancer treatments.
A study – which was published in the Proceedings of the National Academy of Sciences – focuses on the gene SRC-3, found in a type of immune cell known as regulatory T cells (Tregs).
Results from the animal-based study, conducted by Baylor College of Medicine, showed that eliminating the SRC-3 gene in these cells initiated an enduring anticancer response, which removed the tumours entirely.
The results did not present any of the conventional side-effects usually associated with cancer treatments.
“These experiments are preclinical and done in mice – but nonetheless, they are spectacular in outcome," Dr Bert O'Malley, chancellor and professor of molecular and cellular biology at Baylor, told The National. "Human studies will only be done in the future after full FDA [US Food and Drug Administration] approval." Transferring Tregs without the SRC-3 gene to animals with breast cancer tumours also prompted long-term elimination of the tumour, again without negative side-effects.
These promising outcomes have prompted the team to propose further research to evaluate the potential of this method in treating human diseases.
“More than 30 years ago, my lab discovered a protein we called steroid receptor coactivator (SRC) that is required for the effective regulation of gene activity," Dr O'Malley said.
“Over time, we found that a family of SRCs, including SRC-1, SRC-2 and SRC-3, regulate a variety of cellular functions.”
Dr O'Malley's team has shown a specific interest in SRC-3 for its significant role in cancer growth.
It is highly expressed in all human cancers and prominently present in Tregs, which regulate the immune response to cancer.
Through generating mice with a targeted removal of the SRC-3 gene in Tregs, researchers were able to compare the progress of breast cancer in these animals to that in mice still retaining the SRC-3 gene.
Dr O'Malley explained the method of eliminating SRC-3 from regulatory T cells.
“We will delete the gene from 'purified Treg cells' obtained from blood of patients and delete the single gene using Crispr [Clustered regularly interspaced short palindromic repeats] technology," he said.
"The deleted Treg cells will then be transferred back into patients. No harm [will be done] to other cells or to [the] body.
“We were surprised by the results. Breast tumours were eradicated in the SRC-3 knockouts. A subsequent injection of additional cancer cells in these mice did not give rise to new tumours.
“Transferring these cells to animals with pre-existing breast tumours also resulted in cancer eradication. We obtained similar results with prostate cancer.”
Dr O'Malley explained the potential broad application for the findings.
“It is amazingly broad. Our unpublished data shows it works similarly in pancreatic and brain cancers, two currently untreatable cancers,” he said.
The team discovered that Tregs lacking SRC-3 effectively modified the environment surrounding the tumour, helping with its elimination, and instigated a prolonged tumour eradication response.
On closer examination, the researchers found that these modified Tregs proliferated extensively and preferentially infiltrated breast tumours.
Inside the tumour, they released compounds that stimulated an immune response, promoting the entry of other immune cells, such as T cells and natural killer cells, that directly attacked the tumour.
Risks and implications
Dr O'Malley told The National: “The 'Deleted Tregs' do exactly as we hoped, infiltrating only tumours to effect therapeutic tumour destruction.
“There are no risks to normal tissues.”
With regards to the study's implications for long-lasting protection against cancer recurrence, Dr O'Malley told The National: “In animals, after a single cell treatment, the protection is lifelong.
“This approach is likely to synergise with other immunotherapies or chemotherapy.
“No other therapies do this over such a long period of time in mice. We hope it is similar in humans, when this is tried after FDA approval.”
Dr O'Malley also shared an estimated timeline for moving the research into human trials.
“The FDA will require additional studies. We expect to be in human trials in 2024,” he said.
Dr Sang Jun Han, the study's first author, said: “Our findings in animal models are the first to show that Tregs lacking SRC-3 eradicate established cancer tumours and appear to confer long-lasting protection against recurrence.
"We are very excited about the results. All together, they warrant continuing our investigations to translate the findings into a novel, more effective and longer-lasting cancer therapy.”
A study – which was published in the Proceedings of the National Academy of Sciences – focuses on the gene SRC-3, found in a type of immune cell known as regulatory T cells (Tregs).
Results from the animal-based study, conducted by Baylor College of Medicine, showed that eliminating the SRC-3 gene in these cells initiated an enduring anticancer response, which removed the tumours entirely.
The results did not present any of the conventional side-effects usually associated with cancer treatments.
“These experiments are preclinical and done in mice – but nonetheless, they are spectacular in outcome," Dr Bert O'Malley, chancellor and professor of molecular and cellular biology at Baylor, told The National. "Human studies will only be done in the future after full FDA [US Food and Drug Administration] approval." Transferring Tregs without the SRC-3 gene to animals with breast cancer tumours also prompted long-term elimination of the tumour, again without negative side-effects.
These promising outcomes have prompted the team to propose further research to evaluate the potential of this method in treating human diseases.
“More than 30 years ago, my lab discovered a protein we called steroid receptor coactivator (SRC) that is required for the effective regulation of gene activity," Dr O'Malley said.
“Over time, we found that a family of SRCs, including SRC-1, SRC-2 and SRC-3, regulate a variety of cellular functions.”
Dr O'Malley's team has shown a specific interest in SRC-3 for its significant role in cancer growth.
It is highly expressed in all human cancers and prominently present in Tregs, which regulate the immune response to cancer.
Through generating mice with a targeted removal of the SRC-3 gene in Tregs, researchers were able to compare the progress of breast cancer in these animals to that in mice still retaining the SRC-3 gene.
Dr O'Malley explained the method of eliminating SRC-3 from regulatory T cells.
“We will delete the gene from 'purified Treg cells' obtained from blood of patients and delete the single gene using Crispr [Clustered regularly interspaced short palindromic repeats] technology," he said.
"The deleted Treg cells will then be transferred back into patients. No harm [will be done] to other cells or to [the] body.
“We were surprised by the results. Breast tumours were eradicated in the SRC-3 knockouts. A subsequent injection of additional cancer cells in these mice did not give rise to new tumours.
“Transferring these cells to animals with pre-existing breast tumours also resulted in cancer eradication. We obtained similar results with prostate cancer.”
Dr O'Malley explained the potential broad application for the findings.
“It is amazingly broad. Our unpublished data shows it works similarly in pancreatic and brain cancers, two currently untreatable cancers,” he said.
The team discovered that Tregs lacking SRC-3 effectively modified the environment surrounding the tumour, helping with its elimination, and instigated a prolonged tumour eradication response.
On closer examination, the researchers found that these modified Tregs proliferated extensively and preferentially infiltrated breast tumours.
Inside the tumour, they released compounds that stimulated an immune response, promoting the entry of other immune cells, such as T cells and natural killer cells, that directly attacked the tumour.
Risks and implications
Dr O'Malley told The National: “The 'Deleted Tregs' do exactly as we hoped, infiltrating only tumours to effect therapeutic tumour destruction.
“There are no risks to normal tissues.”
With regards to the study's implications for long-lasting protection against cancer recurrence, Dr O'Malley told The National: “In animals, after a single cell treatment, the protection is lifelong.
“This approach is likely to synergise with other immunotherapies or chemotherapy.
“No other therapies do this over such a long period of time in mice. We hope it is similar in humans, when this is tried after FDA approval.”
Dr O'Malley also shared an estimated timeline for moving the research into human trials.
“The FDA will require additional studies. We expect to be in human trials in 2024,” he said.
Dr Sang Jun Han, the study's first author, said: “Our findings in animal models are the first to show that Tregs lacking SRC-3 eradicate established cancer tumours and appear to confer long-lasting protection against recurrence.
"We are very excited about the results. All together, they warrant continuing our investigations to translate the findings into a novel, more effective and longer-lasting cancer therapy.”
Source: https://www.thenationalnews.com
Tags :
Previous Story
- Microsoft signs Xbox game deal with Boosteroid cloud...
- War-themed video game fuels wave of misinformation
- UAE among top five countries for gaming influencers
- Sega builds 'world’s fastest gaming PC' and giving...
- PC Displays May Get Cheaper as Sales Slow
- AMD Ryzen 7 5800X Drops to All-Time Low...
- GeForce RTX 3070 Holiday Deals: Where to Find...
- Core i5-12400F Shows Strong Gaming Performance in New...